Success with iPSC therapies starts earlier than you think. Learn why strategic CMC planning from day one is critical to avoiding costly setbacks in development and GMP manufacturing.
Jul 15, 2025
Developing iPSC Therapies: Why Your CMC Strategy Needs to Start Early
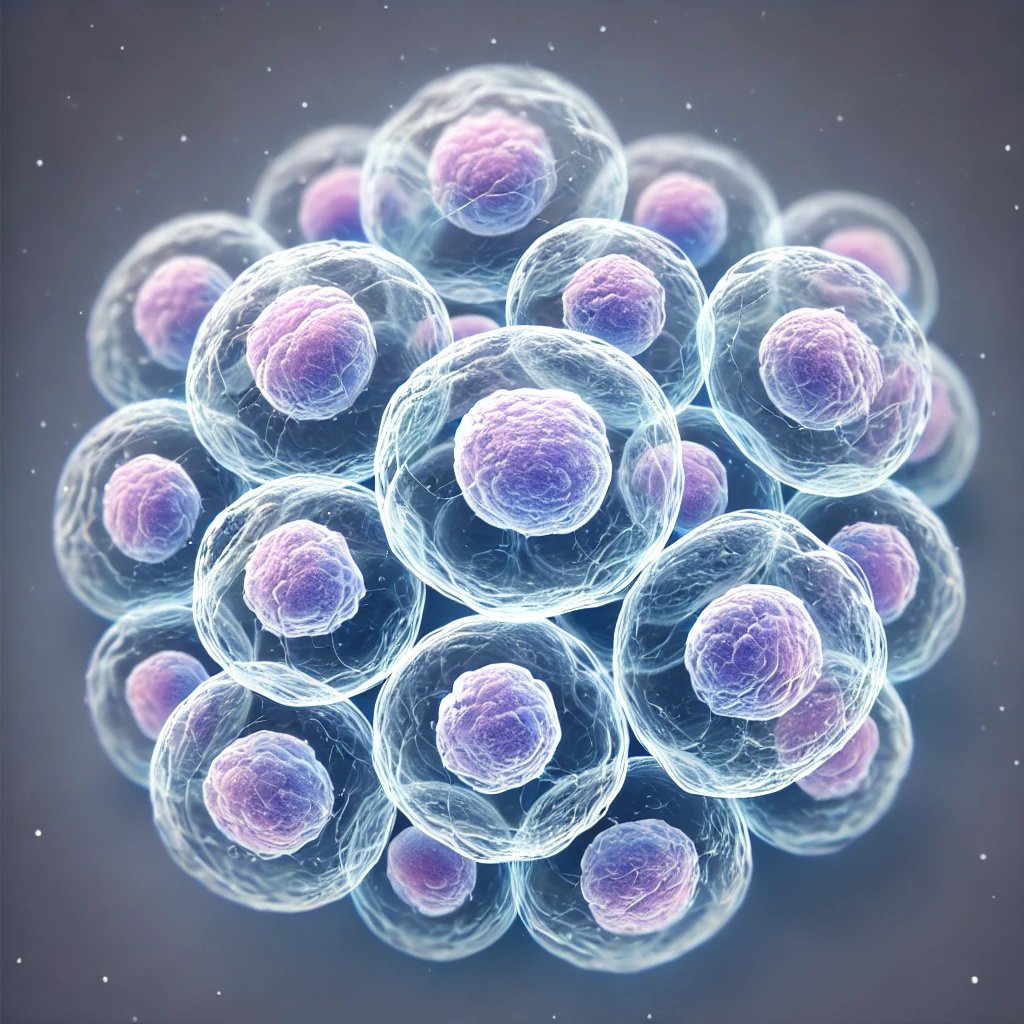
Cell and gene therapies derived from induced pluripotent stem cells (iPSCs) hold remarkable promise for developers, especially those working on early-stage iPSC therapy development. Despite nearly two decades of academic progress since the first iPSCs were developed in 2006, no therapy has yet reached commercialisation. There are many reasons for this, but a recurring theme is that early-stage decisions often set programmes on a difficult trajectory.
From regulatory uncertainty to process variability, iPSC-based cell and gene therapies challenge the assumptions and systems that many developers rely on. That is why your Chemistry, Manufacturing and Controls (CMC) strategy needs to be defined early, not as a box-ticking exercise for a later phase, but as a foundation for long-term viability.
Regulatory ambiguity: principles vs practice
As Drew Hope, Senior Compliance Consultant and UK QP at eXmoor Pharma, explains, “One of the key issues is inconsistent regulatory expectations around GMP. While some authorities, such as the Paul Ehrlich Institute in Germany, require full GMP compliance from the moment of cell procurement, others, including the MHRA and FDA, take a more flexible stance. They allow for earlier-stage work to take place under ‘GMP principles’ provided quality risks are well documented and controlled.”
iPSC regulatory strategy remains a moving target across regions. “The assumption that an R&D-derived iPSC line will be accepted is one of the most common and costly mistakes we see,” says Hope. There is no global consensus on what’s acceptable. If a developer plans for one regulatory route and later needs to access another market, they may face the expense of starting over.
Early risk assessments and documentation of all processing steps, even at the research stage, are essential. But as Hope adds, “Many developers do not realise this until their timelines or investment depend on it.”
Process complexity: no one-size-fits-all

“There isn’t a gold-standard process for iPSC manufacturing yet. Most platforms are still being adapted from other technologies, and the target cell type defines everything from reagents to culture conditions.”
From a technical standpoint, iPSC-based cell and gene therapies are inherently more variable than other CGTs. As Adam Janvier, eXmoor’s Head of Cell Therapy, explains, “There isn’t a gold-standard process for iPSC manufacturing yet. Most platforms are still being adapted from other technologies, and the target cell type defines everything from reagents to culture conditions.”
This is because iPSCs are pluripotent. They can become many different types of cells, each with unique differentiation pathways and culture needs. A single iPSC line might support the development of photoreceptors, hepatocytes, macrophages or regulatory T cells across different programmes. That means processes cannot be easily standardised, and developers must design flexible platforms from the outset.
“Even at the bioreactor level, scale-up is constrained by the fragility of iPSC aggregates. We are retrofitting fermentation vessels that were designed for microbes or vectors,” Janvier notes. “But iPSCs are shear-sensitive and genetically less stable. The bigger the vessel, the harder it is to manage the mechanical forces without harming the cells.”
New bioreactor designs are emerging, but until they become widespread, these constraints must be anticipated during early process development.
Analytics: the earlier, the better
In early-stage iPSC manufacturing, assay development and characterisation are often underestimated. “There is no single regulatory definition of what iPSCs should be tested for,” Janvier explains. Most guidelines suggest approaches, but they are not definitive. That makes early analytical planning even more important.
Key considerations include:
- Selecting relevant markers for flow cytometry
- Establishing robust genetic stability assays
- Documenting and validating differentiation endpoints
Too often, clients arrive with limited data or assumptions based on academic workflows. If the analytical package is not well defined, you cannot scale or transfer the process with confidence, says Janvier. It creates risk that should have been avoided.
Early input from regulatory and translational experts helps shape a realistic testing plan, one that not only satisfies current needs but can evolve with regulatory expectations.
GMP readiness: bridging development and manufacturing
The key to GMP readiness lies in two areas: planning and executing the technology transfer stages of both the iPSC process and associated analytics, and training of the GMP and QC teams.
1. Planning and execution of technology transfer
For iPSCs, it is critical that both the cell therapy process and associated analytical methods are transferred in a structured and well-documented manner. Because iPSCs are pluripotent, it is essential that the Critical Process Parameters (CPPs) required to ensure successful differentiation into the intended cell type are clearly defined and fully specified for execution in GMP manufacture. If these CPPs are poorly characterised, the process may fail to deliver cells with the required phenotype and functionality. This risk becomes especially significant when aiming for batch release.
Embedding process development experts within the GMP team helps maintain continuity and ensures that detailed knowledge of the differentiation pathway and its tolerances is transferred effectively. As Gillian Lewis, GMP QP at eXmoor Pharma, explains, “For iPSCs, understanding the link between process conditions and cell fate is critical. That knowledge must be preserved and fully integrated into GMP operations.”
2. Training of the GMP and QC teams
Early training of the GMP and QC teams is essential. Providing operators and analysts with sufficient lead time to become familiar with the process helps build confidence in execution, enables early issue identification, and ensures that analytics are supported by a capable and informed QC function.
Lewis continues: “GMP facilities must also be adapted to the specific requirements of iPSC manufacturing. These processes often involve long-duration cultures and partially open steps, requiring sustained aseptic technique and facility layouts that support extended activity times. While closed systems are ideal, they are not always achievable, particularly in early-phase manufacturing.”
GMP success ultimately depends on how early the manufacturing team is involved and how well process knowledge is carried forward into GMP execution.
Rethink the starting line
As Hope reflects, “The point of failure in many iPSC programmes is not GMP. It is what happened, or did not happen, long before that.” Whether the barrier is a regulator’s definition of GMP, an inconsistent differentiation protocol, or missing analytical data, the lesson is the same: late-stage fixes cannot solve early-stage problems.
Success depends not just on when you act, but on how well critical knowledge is carried from development into manufacturing. That includes analytical methods, process parameters and the expertise required to execute them consistently at GMP.
Developers working with iPSCs must take a strategic, integrated approach from the outset. That means involving regulatory consultants, process engineers, analytical experts and GMP teams early, not when clinical material is already in sight.
Developing an iPSC-based therapy? See how we help de-risk your CMC and regulatory strategy from day one by exploring our iPSC capabilities.
Latest News
Let’s Accelerate Your Therapy Together
Whether you're in early-stage development or scaling up for commercial production, eXmoor Pharma provides the expertise and flexibility you need. Partner with us to move your therapy forward with confidence.



